Results for “half doses” 45 found
The Story of VaccinateCA
The excellent Patrick McKenzie tells the story of VaccineCA, the ragtag group of volunteers that quickly became Google’s and then the US Government’s best source on where to find vaccines during the pandemic.
Wait. The US Government was giving out the vaccines. How could they not know where the vaccines were? It’s complicated. Operation Warp Speed delivered the vaccines to the pharmacy programs and to the states but after that they dissappeared into a morass of incompatible systems.
[L]et’s oversimplify: Vials were allocated by the federal government to states, which allocated them to counties, which allocated them to healthcare providers and community groups. The allocators of vials within each supply chain had sharply limited ability to see true systemic supply levels. The recipients of the vials in many cases had limited organizational ability to communicate to potential patients that they actually had them available.
Patients then asked the federal government, states, counties, healthcare providers and community groups, ‘Do you have the vaccine?’ And in most cases the only answer available to the person who picked up the phone was ‘I don’t have it. I don’t know if we have it. Plausibly someone has it. Maybe you should call someone else.’ Technologists will see the analogy to a distributed denial of service incident, and as if the overwhelming demand was not enough of a problem, the rerouting of calls between institutions amplified the burden on the healthcare system. Vaccine seekers were routinely making dozens of calls.
This caused a standing wave of inquiries to hit all levels of US healthcare infrastructure in the early months of the vaccination effort. Very few of those inquiries went well for any party. It is widely believed, and was widely believed at the time, that this was primarily because supply was lacking, but it was often the case that supply was frequently not being used as quickly as it was produced because demand could not find it.
It turned out that the best way to get visibility into this mess was not to trace the vaccines but to call the endpoints on the phone and then create a database that people could access which is what VaccinateCA did but in addition to finding the doses they had to deal with the issue of who was allowed access.
A key consideration for us, from the first day of the effort, was recording not just which pharmacist had vials but who they thought they could provide care to. This was dependent on prevailing regulations in their state and county, interpretations of those regulations by the pharmacy chain, and (frequently!) ad hoc decision-making by individual medical providers. Individual providers routinely made decisions that the relevant policy makers did not agree comported with their understanding of the rules.
VaccinateCA saw the policy sausage made in real time in California while keeping an eye on it nationwide. It continues to give me nightmares.
California, not to mince words, prioritized the appearance of equity over saving lives, over and over and over again, as part of an explicitly documented strategy, at all levels of the government. You can read the sanitized version of the rationale, by putative medical ethics experts, in numerous official documents. The less sanitized version came out frequently in meetings.
This was the official strategy.
The unofficial strategy, the result the system actually obtained, was that early access to the vaccine was preferentially awarded based on proximity to power and to the professional-managerial class.
… The essential workers list heavily informed the vaccination prioritization schedule. Lobbyists used it as procedural leverage to prioritize their clients for vaccines. The veterinary lobby was unusually candid, in writing, about how it achieved maximum priority (1A) for veterinarians due to them being ‘healthcare workers’.
Teachers’ unions worked tirelessly and landed teachers a 1B. They were ahead of 1C, which included (among others) non-elderly people for whom preexisting severe disability meant that ‘a covid-19 infection is likely to result in severe life-threatening illness or death’. The public rationale was that teachers were at elevated risk of exposure through their occupation. Schools were, of course, mostly closed at the time, and teachers were Zooming along with the rest of the professional-managerial class, but teachers’ unions have power and so 1B it was. Young, healthy teachers quarantining at home were offered the vaccine before people who doctors thought would probably die if they caught Covid.
Now repeat this exercise up and down the social structure and economy of the United States.
…Healthcare providers were fired for administering doses that were destined to expire uselessly. The public health sector devoted substantial attention to the problem of vaccinating too many people during a pandemic. Administration of the formal spoils system became farcically complicated and frequently outcompeted administration of the vaccine as a goal.
The process of registering for the vaccine inherited the complexity of the negotiation over the prioritization, and so vulnerable people were asked to parse rules that routinely befuddled healthy professional software engineers and healthcare administrators – the state of New York subjected senior citizens to a ‘51 step online questionnaire that include[d] uploading multiple attachments’!
That isn’t hyperbole! New York meant to do that! On purpose!
Lives were sacrificed by the thousands and tens of thousands for political reasons. Many more were lost because institutions failed to execute with the competence and vigor the United States is abundantly capable of.
…The State of California instituted a policy of redlining in the provision of medical care in a pandemic to thunderous applause from its activist class and medical ethics experts….Residency restrictions were pervasively enforced at the county level and frequently finer-grained than that. A pop-up clinic, for example, might have been restricted to residents of a single zip code or small group of zip codes.
All people are equal in the eyes of the law in California, but some people are . . . let’s politely say ‘administratively disfavored’.
The theory was, and you could write down this part of it, disfavored potential patients might use social advantages like better access to information and transportation to present themselves for treatment at locations that had doses allocated for favored potential patients. This part of the theory was extremely well-founded. Many people were willing to drive the length and breadth of California for their dose and did so.
What many wanted to do, and this is the part that they couldn’t write down, is deny healthcare to disfavored patients. Since healthcare providers are public accommodations in the state of California, they are legally forbidden from discriminating on the basis of characteristics that some people wanted to discriminate on. So that was laundered through residency restrictions.
Many more items of interest. I didn’t know this incredibly fact about the Biden adminsitratins Vaccines.gov for example:
Pharmacies through the FRPP had roughly half of the doses; states and counties had roughly the other half (sometimes administered at pharmacies, because clearly this isn’t complicated enough yet). You would hope that state and county doses were findable on Vaccines.gov. It was going to be the centerpiece of the Biden administration’s effort to fix the vaccine finding problem and take credit for doing so.
…Since the optics would be terrible if America appeared to serve some states much better than others on the official website that everyone would assume must show all the doses, no state doses, not even from states that would opt in, would be shown on it, at least not at the moment of maximum publicity. Got that?
A good point about America.
We also benefited from another major strength of America: You cannot get arrested, jailed, or shot for publishing true facts, even if those facts happen to embarrass people in positions of power. Many funders wanted us to expand the model to a particular nation. In early talks with contacts there in civil society, it was explained repeatedly and at length that a local team that embarrassed the government’s vaccination rollout would be arrested and beaten by people carrying guns. This made it ethically challenging to take charitable donations and try to recruit that team.
Many more points of interest about the process of running a medical startup during a pandemic. Read the whole thing.
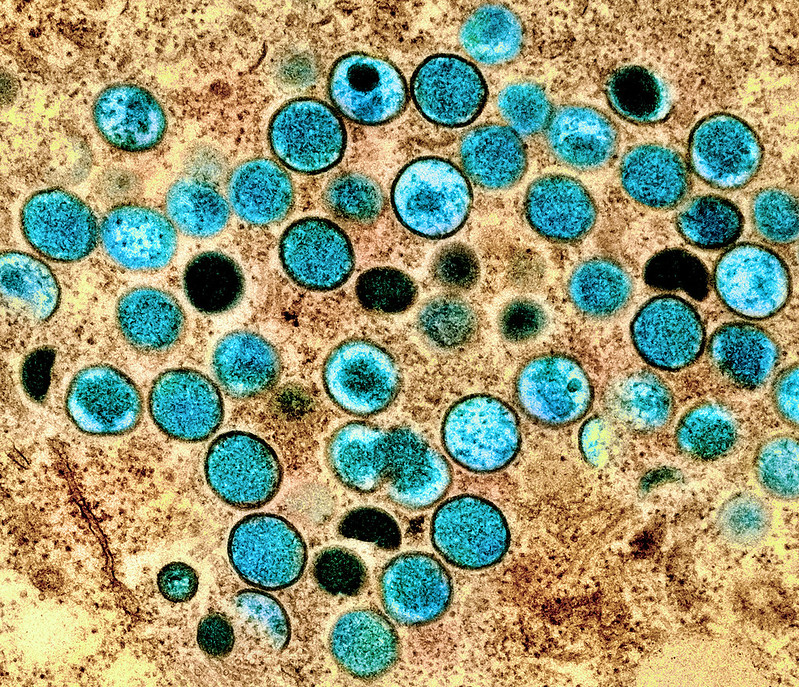
Dose Stretching for the Monkeypox Vaccine
We are making all the same errors with monkeypox policy that we made with Covid but we are correcting the errors more rapidly. (It remains to be seen whether we are correcting rapidly enough.) I’ve already mentioned the rapid movement of some organizations to first doses first for the monkeypox vaccine. Another example is dose stretching. I argued on the basis of immunological evidence that A Half Dose of Moderna is More Effective Than a Full Dose of AstraZeneca and with Witold Wiecek, Michael Kremer, Chris Snyder and others wrote a paper simulating the effect of dose stretching for COVID in an SIER model. We even worked with a number of groups to accelerate clinical trials on dose stretching. Yet, the idea was slow to take off. On the other hand, the NIH has already announced a dose stretching trial for monkeypox.
Scientists at the National Institutes of Health are getting ready to explore a possible work-around. They are putting the finishing touches on the design of a clinical trial to assess two methods of stretching available doses of Jynneos, the only vaccine in the United States approved for vaccination against monkeypox.
They plan to test whether fractional dosing — using one-fifth of the regular amount of vaccine per person — would provide as much protection as the current regimen of two full doses of the vaccine given 28 days apart. They will also test whether using a single dose might be enough to protect against infection.
The first approach would allow roughly five times as many people to be vaccinated as the current licensed approach, and the latter would mean twice as many people could be vaccinated with existing vaccine supplies.
…The answers the study will generate, hopefully by late November or early December, could significantly aid efforts to bring this unprecedented monkeypox outbreak under control.
Another interesting aspect of the dose stretching protocol is that the vaccine will be applied to the skin, i.e. intradermally, which is known to often create a stronger immune response. Again, the idea isn’t new, I mentioned it in passing a couple of times on MR. But we just weren’t prepared to take these step for COVID. Nevertheless, COVID got these ideas into the public square and now that the pump has been primed we appear to be moving more rapidly on monkeypox.
Addendum: Jonathan Nankivell asked on the prediction market, Manifold Markets, ‘whether a 1/5 dose of the monkey pox vaccine would provide at least 50% the protection of the full dose?’ which is now running at a 67% chance. Well worth doing the clinical trial! Especially if we think that the supply of the vaccine will not expand soon.
How many times are we going to make this kind of mistake?
The shortage of vaccines to combat a fast-growing monkeypox outbreak was caused in part because the Department of Health and Human Services failed early on to ask that bulk stocks of the vaccine it already owned be bottled for distribution, according to multiple administration officials familiar with the matter.
By the time the federal government placed its orders, the vaccine’s Denmark-based manufacturer, Bavarian Nordic, had booked other clients and was unable to do the work for months, officials said — even though the federal government had invested well over $1 billion in the vaccine’s development.
The government is now distributing about 1.1 million doses, less than a third of the 3.5 million that health officials now estimate are needed to fight the outbreak. It does not expect the next delivery, of half a million doses, until October. Most of the other 5.5 million doses the United States has ordered are not scheduled to be delivered until next year, according to the federal health agency.
Here is more from the NYT.
Fractional Dosing Trials
My paper Testing fractional doses of COVID-19 Vaccines, co-authored with Kremer et al., has now been published at PNAS. I covered the paper in A Half Dose of Moderna is More Effective than A Full Dose of Astra Zeneca and other posts so I won’t belabor the basic ideas. One new point is that thanks to the indefatigable Michael Kremer and the brilliant Witold Wiecek, clinical trials on fractional dosing on a large scale have begun in Nigeria. Here are a few key points:
WHO SAGE Outreach: The authors have met and presented their work to the World Health Organization (WHO) Strategic Advisory Group of Experts on Immunization (SAGE), with follow-up meetings to present evidence coming from new studies.
DIL Workshop and Updates: In the fall of 2021, the Development Innovation Lab (DIL) at UChicago, led by Professor Kremer, hosted a workshop on fractional dosing, collecting updates from clinical researchers from multiple countries conducting fractional dosing trials for COVID-19 vaccines. The workshop also covered issues relating to trial design and included participants from Belgium, Brazil, Ghana, the Netherlands, Nigeria, Thailand, South Africa, UK and the US.
CEPI Outreach: Professor Kremer has also presented this research to The Coalition for Epidemic Preparedness Innovations (CEPI), which is now pursuing a platform trial of fractional dosing.
Country Trials – Nigeria: With the support of DIL and the research team and generous support and advice from WAM Foundation, the charitable arm of Weiss Asset Management and Open Philanthropy, a trial is being conducted in Nigeria by the Nigerian Institute of Medical Research, National Institute of Pharmaceutical Research and Development, National Agency for Food and Drug Administration and Control, and the National Primary Health Care Development Agency, in coordination with the Federal Ministry of Health.
A comprehensive list of all the trials on fractional dosing conducted to date is at the link. Fractional dosing may come too late for COVID-19 vaccines but perhaps next time a shortage of a vaccine looms we will be more quick to consider policies to stretch supplies.
Is “wrestled” the right word here?
The advisers also wrestled with the practicalities of endorsing a booster shot for only Pfizer-BioNTech recipients, when close to half of vaccinated Americans have received Moderna or J. & J. vaccines.
“I just don’t understand how, later this afternoon, we can say to people 65 and older, ‘You’re at risk for severe disease and death, but only half of you can protect yourselves right now,’” said Dr. Sarah Long, a pediatrician and infectious diseases expert at Drexel University College of Medicine in Pennsylvania.
I feel I do understand how, though of course I do not approve. Here is more from the NYT. And for a further multi-cocktail blitz of what I can only call immoral insanity:
Committee members also expressed concern on Thursday that some recommendations — particularly that certain younger Americans be allowed booster shots after an assessment of individual risks — would mean that only the wealthy and educated would gain access to additional shots.
Better that no one get such doses? Maybe so, just read further:
Some experts seemed to suggest on Wednesday that it might be better to hold off on recommending any booster shots until recipients of all three vaccines could qualify for them.
Still a train wreck, the whole thing. At least the CDC head has had the guts to override the vaccine panel. Of course there is no single way to get it right with a few rules, so how about injecting a greater dose of individual choice? Or do they need to make a special rule letting people in vaccine-shy Kentucky get boosters too?
What’s the Right Dose for Boosters?
The Biden administration says booster shots are coming, but the FDA hasn’t decided on the dose. Moderna wants a half-shot booster. Pfizer a full shot. But could the best dose for Americans and for the world be even less?
COVID-19 vaccines are the first successful use of mRNA vaccine technology, so a lot remains unknown. But identifying the smallest dose needed to provide effective boosting is critical to protect Americans from adverse effects, increase confidence in vaccines, and mitigate global vaccine inequity.
We’ve known since earlier this year that a half-dose of the Moderna vaccine produces antibody levels similar to the standard-dose and newer information suggests that even a quarter-dose vaccine may do the same. If a half or quarter dose is nearly as effective as a standard dose for first and second shots then a full dose booster may well be an overdose. The essential task of a booster is to “jog” the immune system’s memory of what it’s supposed to fight. Data from the world of hepatitis B suggest that the “reminder” need not be as intense as the initial “lesson.” And in the cases of tuberculosis, meningitis, and yellow fever vaccines, lower doses have been as good or better than the originals.
Lower doses could also reduce risks of adverse effects.
That’s myself and physicians Garth Strohbehn and William F. Parker on the Med Page Today. Strohbehn is an oncologist and specialist in optimizing doses for cancer drugs. William Parker is a pulmonologist and professor of medicine at the University of Chicago.
Book Review: Andy Slavitt’s Preventable
Like Michael Lewis’s The Premonition which I reviewed earlier, Andy Slavitt’s Preventable is a story of heroes, only all the heroes are named Andy Slavitt. It begins, as all such stories do, with an urgent call from the White House…the President needs you now! When not reminding us (e.g. xv, 14, 105, 112, 133, 242, 249) of how he did “nearly the impossible” and saved Obamacare he tells us how grateful other people were for his wise counsel, e.g. “Jared Kushner’s name again flashed on my phone. I picked up, and he was polite and appreciative of my past help.” (p.113), “John Doer was right to challenge me to make my concerns known publicly. Hundreds of thousands of people were following my tweets…” (p. 55)
Slavitt deserves praise for his work during the pandemic so I shouldn’t be so churlish but Preventable is shallow and politicized and it rubbed me the wrong way. Instead of an “inside account” we get little more than a day-by-day account familiar to anyone who lived through the last year and half. Slavitt rarely departs from the standard narrative.
Trump, of course, comes in for plenty of criticism for his mishandling of the crisis. Perhaps the most telling episode was when an infected Trump demanded a publicity jaunt in a hermetically sealed car with Secret Service personnel. Trump didn’t care enough to protect those who protected him. No surprise he didn’t protect us.
The standard narrative, however, leads Slavitt to make blanket assertions—the kind that everyone of a certain type knows to be true–but in fact are false. He writes, for example:
In comparison to most of these other countries, the American public was impatient, untrusting, and unaccustomed to sacrificing individual rights for the public good. (p. 65)
Data from the Oxford Coronavirus Government Response Tracker (OxCGRT) show that the US “sacrifice” as measured by the stringency of the COVID policy response–school closures; workplace closures; restrictions on public gatherings; restrictions on internal movements; mask requirements; testing requirements and so forth–was well within the European and Canadian average.
The pandemic and the lockdowns split Americans from their friends and families. Birthdays, anniversaries, even funerals were relegated to Zoom. Jobs and businesses were lost in the millions. Children couldn’t see their friends or even play in the park. Churches and bars were shuttered. Music was silenced. Americans sacrificed plenty.

Some of Slavitt’s assertions are absurd.
The U.S. response to the pandemic differed from the response in other parts of the world largely in the degree to which the government was reluctant to interfere with our system of laissez-faire capitalism…
Laissez-faire capitalism??! Political hyperbole paired with lazy writing. It would be laughable except for the fact that such hyperbole biases our thinking. If you read Slavitt uncritically you’d assume–as Slavitt does–that when the pandemic hit, US workers were cast aside to fend for themselves. In fact, the US fiscal response to the pandemic was among the largest and most generous in the world. An unemployed minimum wage worker in the United States, for example, was paid a much larger share of their income during the pandemic than a similar worker in Canada, France, or Germany (and no, that wasn’t because the US replacement rate was low to begin with.)

This is not to deny that low-wage workers bore a larger brunt of the pandemic than high-wage workers, many of whom could work from home. Slavitt implies, however, that this was a “room-service pandemic” in which the high-wage workers demanded a reopening of the economy at the expense of low-wage workers. As far as the data indicate, however, the big divisions of opinion were political and tribal not by income per se. The Washington Post, for example, concluded:
There was no significant difference in the percentage of people who said social distancing measures were worth the cost between those who’d seen no economic impact and those who said the impacts were a major problem for their households. Both groups broadly support the measures.
Perhaps because Slavitt believes his own hyperbole about a laissez-faire economy he can’t quite bring himself to say that Operation Warp Speed, a big government program of early investment to accelerate vaccines, was a tremendous success. Instead he winds up complaining that “even with $1 billion worth of funding for research and development, Moderna ended up selling its vaccine at about twice the cost of an influenza vaccine.” (p. 190). Can you believe it? A life-saving, economy-boosting, pandemic ending, incredibly-cheap vaccine, cost twice as much as the flu vaccine! The horror.
Slavitt’s narrative lines up “scientific experts” against “deniers, fauxers, and herders” with the scientific experts united on the pro-lockdown side. Let’s consider. In Europe one country above all others followed the Slavitt ideal of an expert-led pandemic response. A country where the public health authority was free from interference from politicians. A country where the public had tremendous trust in the state. A country where the public were committed to collective solidarity and the public welfare. That country, of course, was Sweden. Yet in Sweden the highly regarded Public Health Agency, led by state epidemiologist Anders Tegnell, an expert in infectious diseases who had directed Sweden’s response to the swine flu epidemic, opposed lockdowns, travel restrictions, and the general use of masks.
Moreover, the Public Health Agency of Sweden and Tegnell weren’t a bizarre anomaly, anti-lockdown was probably the dominant expert position prior to COVID. In a 2006 review of pandemic policy, for example, four highly-regarded experts argued:
It is difficult to identify circumstances in the past half-century when large-scale quarantine has been effectively used in the control of any disease. The negative consequences of large-scale quarantine are so extreme (forced confinement of sick people with the well; complete restriction of movement of large populations; difficulty in getting critical supplies, medicines, and food to people inside the quarantine zone) that this mitigation measure should be eliminated from serious consideration.
Travel restrictions, such as closing airports and screening travelers at borders, have historically been ineffective.
….a policy calling for communitywide cancellation of public events seems inadvisable.
The authors included Thomas V. Inglesby, the Director of the Johns Hopkins Center for Health Security, one of the most highly respected centers for infectious diseases in the world, and D.A. Henderson, the legendary epidemiologist widely credited with eliminating smallpox from the planet.
Tegnell argued that “if other countries were led by experts rather than politicians, more nations would have policies like Sweden’s” and he may have been right. In the United States, for example, the Great Barrington declaration, which argued for a Swedish style approach and which Slavitt denounces in lurid and slanderous terms, was written by three highly-qualified, expert epidemiologists; Martin Kulldorff from Harvard, Sunetra Gupta from Oxford and Jay Bhattacharya from Stanford. One would be hard-pressed to find a more expert group.
The point is not that we should have followed the Great Barrington experts (for what it is worth, I opposed the Great Barrington declaration). Ecclesiastes tells us:
… that the race is not to the swift, nor the battle to the strong, neither yet bread to the wise, nor yet riches to men of understanding, nor yet favor to men of skill; but time and chance happeneth to them all.
In other words, the experts can be wrong. Indeed, the experts are often divided, so many of them must be wrong. The experts also often base their policy recommendations on factors beyond their expertise, including educational, class, and ideological biases, so the experts are to be trusted more on factual questions than on ethical answers. Nevertheless, the experts are more likely to be right than the non-experts. So how should one navigate these nuances in a democratic society? Slavitt doesn’t say.
Slavitt’s simple narrative–Trump bad, Biden good, Follow the Science, Be Kind–can’t help us as we try to improve future policy. Slavitt ignores most of the big questions. Why did the CDC fail in its primary mission? Indeed, why did the CDC often slow our response? Why did the NIH not quickly fund COVID research giving us better insight on the virus and its spread? Why were the states so moribund and listless? Why did the United States fail to adopt first doses first, even though that policy successfully saved lives by speeding up vaccinations in Great Britain and Canada?
To the extent that Slavitt does offer policy recommendations they aren’t about reforming the CDC, FDA or NIH. Instead he offers us a tired laundry list; a living wage, affordable housing, voting reform, lobbying reform, national broadband, and reduction of income inequality. Surprise! The pandemic justified everything you believed all along! But many countries with these reforms performed poorly during the pandemic and many without, such as authoritarian China, performed relatively well. All good things do not correlate.
Trump’s mishandling of the pandemic make it easy to blame him and call it a day. But the rot is deep. If we do not get to the core of our problems we will not be ready for the next emergency. If we are lucky, we might face the next emergency with better leadership but a great country does not rely on luck.
More on Alternative Dosing
Some quick comments in response to questions and discussion about my paper Could Vaccine Dose Stretching Reduce COVID-19 Deaths? (written with the all-star cast of Witold Więcek, Amrita Ahuja, Michael Kremer, Alexandre Simoes Gomes, Christopher M. Snyder and Brandon Joel Tan.
1) Any method of increasing vaccine supply will require other changes in the supply chain such as more needles. We think alternative dosing can increase supply quickly with the fewest supply chain disruptions.
2) If we had started Moderna with 50 ug dosing no one would be advocating for 100 ug dosing, thereby halving supply. Rather than “full” or “half-doses,” which bias thinking, we should talk about alternative dosing and ug.
3) Judging by neutralizing antibodies, a 50 ug dose of, for example, Moderna looks to be more effective than standard dosing of many other vaccines including AZ and J&J and much better than others such as Sinovac. Thus alternative dosing is a way to *increase* the quality of vaccine for many people.
4) A 50 ug dose vaccine available today is much higher quality than a 100 ug dose vaccine available one year from now.
5) There are substantial risks from following the current approach, as India and now parts of Africa illustrate. Alternative dosing has a very large upside but small downside since we could switch back to standard doses. For example, Great Britain and Canada delayed the second dose to 12 and 16 weeks respectively but have since reduced the dosing interval as more supplies have become available.
6) The greatest risk to immune escape comes from the unvaccinated. Alternative dosing protects not only those who are dosed but by reducing transmission also reduces risks to the unvaccinated.
7) The key question we face now is not whether there are objections and complications to alternative dosing (there are) the key question is what additional information, available quickly could resolve the most uncertainty? In other words, what can we learn soon that would most aid decision makers?
See the paper for details and also my previous post, A Half Dose of Moderna is More Effective Than a Full Dose of AstraZeneca.
Addendum: It should be clear that this isn’t about the United States, it is about getting high-quality vaccine to places that have little to none.
Fractional Dosing Trials Now!
Fractional dosing has the potential to massively increase the supply of COVID vaccine. The Moderna Phase I clinical trial and Pfizer Phase I/II trials already indicated a substantial immune response with smaller doses but the vaccine companies are under-incentivized to run additional fractional dosing trials (they won’t gain trillions, at best they will gains billions and might even lose some profit) and governments and private organizations are not picking up the ball. There are just two small trials underway that I am aware of:
- Sciensano, the national public health institute of Belgium, is running a trial on a 2/3rd fractional dose of the Pfizer vaccine. (I think they were previously going to also study Moderna but now seem to have dropped that arm.)
- Johnson and Johnson is trying a .3 mil dose as opposed to a 0.5 mil dose but they haven’t started recruiting.
N.B. now that we know that the vaccines work. we don’t need to study every dosage for efficacy against the virus. Instead of efficacy studies we can study how the vaccine is working in the body compared to those fully immunized, immunogencity trials (which is what the above trials are doing) and then use data and theory to infer effectiveness. If we felt it necessary to study effectiveness, human challenge trials would be ideal in this situation as you can study gradually smaller doses with little risk to the patients. But given the urgency, immunogenicity trials should provide enough information to make decisions on the ground. To limit risk, one could do a half-dose on the second dose or one could do a half-dose in people under the age of 50. Both of these regimens would still create significant increases in supply. Recall that in 2018, facing a yellow fever epidemic and a shortage of vaccine, Brazil used 1/5th doses to break the epidemic.
There are no guarantees but the world is ignoring a potential trillion dollar bill lying on the sidewalk.
Hat tip for discussion: Witold and Amrita.
India Delays the 2nd Dose; Delaying 2nd Dose Improves Immune Response; Fractional Dosing
India has delayed the second dose to 12-16 weeks.
In other news, delaying the second dose of the Pfizer vaccine appears to improves the immune response (as was also found for the AstraZeneca vaccine). The latter is a news report based on a press release so some caution is warranted but frankly this was always the Bayesian bet since most vaccines have a longer time between doses as that helps the immune system. As Tyler and myself both argued, the short gap between the first and second dose was chosen to speed up the clinical trials not to maximize immunity. That was the right decision in the emergency but it was never the case that following the clinical trial regimen was “going by the science” no matter what Fauci said.
Many lives have been lost by not going to first doses first earlier, both here and in India.
Every country should move to a regimen in which the second dose comes at 12-16 weeks, even the United States, as this may improve the immune response and help other countries get a little bit ahead in their vaccine drives.
May I now also beat the drum some more on fractional dosing? Many people (not everyone) report that the second mRNA dose packs a wallop. I suspect that a half dose at 12-16 weeks would be plenty and that would free up significant capacity to vaccinate more people with first doses. We could also run some trials on half-doses for the young as a way to balance dosing and risk. Again this will matter for the rest of the world more than the United States but stretching doses in the United States will help the rest of the world and the arguments against stretching doses are now much diminished.
Patents are Not the Problem!
For the last year and a half I have been shouting from the rooftops, “invest in capacity, build more factories, shore up the supply lines, spend billions to save trillions.” Fortunately, some boffins in the Biden administration have found a better way, “the US supports the waiver of IP protections on COVID-19 vaccines to help end the pandemic.”
Waive IP protections. So simple. Why didn’t I think of that???
Patents are not the problem. All of the vaccine manufacturers are trying to increase supply as quickly as possible. Billions of doses are being produced–more than ever before in the history of the world. Licenses are widely available. AstraZeneca have licensed their vaccine for production with manufactures around the world, including in India, Brazil, Mexico, Argentina, China and South Africa. J&J’s vaccine has been licensed for production by multiple firms in the United States as well as with firms in Spain, South Africa and France. Sputnik has been licensed for production by firms in India, China, South Korea, Brazil and pending EMA approval with firms in Germany and France. Sinopharm has been licensed in the UAE, Egypt and Bangladesh. Novavax has licensed its vaccine for production in South Korea, India, and Japan and it is desperate to find other licensees but technology transfer isn’t easy and there are limited supplies of raw materials:
Virtually overnight, [Novavax] set up a network of outside manufacturers more ambitious than one outside executive said he’s ever seen, but they struggled at times to transfer their technology there amid pandemic travel restrictions. They were kicked out of one factory by the same government that’s bankrolled their effort. Competing with larger competitors, they’ve found themselves short on raw materials as diverse as Chilean tree bark and bioreactor bags. They signed a deal with India’s Serum Institute to produce many of their COVAX doses but now face the realistic chance that even when Serum gets to full capacity — and they are behind — India’s government, dealing with the world’s worst active outbreak, won’t let the shots leave the country.
Plastic bags are a bigger bottleneck than patents. The US embargo on vaccine supplies to India was precisely that the Biden administration used the DPA to prioritize things like bioreactor bags and filters to US suppliers and that meant that India’s Serum Institute was having trouble getting its production lines ready for Novavax. CureVac, another potential mRNA vaccine, is also finding it difficult to find supplies due to US restrictions (which means supplies are short everywhere). As Derek Lowe said:
Abolishing patents will not provide more shaker bags or more Chilean tree bark, nor provide more of the key filtration materials needed for production. These processes have a lot of potential choke points and rate-limiting steps in them, and there is no wand that will wave that complexity away.
Technology transfer has been difficult for AstraZeneca–which is one reason they have had production difficulties–and their vaccine uses relatively well understood technology. The mRNA technology is new and has never before been used to produce at scale. Pfizer and Moderna had to build factories and distribution systems from scratch. There are no mRNA factories idling on the sidelines. If there were, Moderna or Pfizer would be happy to license since they are producing in their own factories 24 hours a day, seven days a week (monopolies restrict supply, remember?). Why do you think China hasn’t yet produced an mRNA vaccine? Hint: it isn’t fear about violating IP. Moreover, even Moderna and Pfizer don’t yet fully understand their production technology, they are learning by doing every single day. Moderna has said that they won’t enforce their patents during the pandemic but no one has stepped up to produce because no one else can.
The US trade representative’s announcement is virtue signaling to the anti-market left and will do little to nothing to increase supply.
What can we do to increase supply? Sorry, there is no quick and cheap solution. We must spend. Trump’s Operation Warp Speed spent on the order of $15 billion. If we want more, we need to spend more and on similar scale. The Biden administration paid $269 million to Merck to retool its factories to make the J&J vaccine. That was a good start. We could also offer Pfizer and Moderna say $100 a dose to produce in excess of their current production and maybe with those resources there is more they could do. South Africa and India and every other country in the world should offer the same (India hasn’t even approved the Pfizer vaccine and they are complaining about IP!??) We should ease up on the DPA and invest more in the supply chain–let’s get CureVac and the Serum Institute what they need. We should work like hell to find a substitute for Chilean tree bark. See my piece in Science co-authored with Michael Kremer et. al. for more ideas. (Note also that these ideas are better at dealing with current supply constraints and they also increase the incentive to produce future vaccines, unlike shortsighted patent abrogation.)
Bottom line is that producing more takes real resources not waving magic patent wands.
You may have gathered that I am angry. I am indeed angry that the people in power think they can solve real problems on the cheap and at someone else’s expense. This is not serious. I am also angry that they are sending the wrong message about business, profits and capitalism. So let me end on positive note. Like the Apollo program and Dunkirk, the creation of the mRNA vaccines by Pfizer and Moderna should be lauded with Nobel prizes and major movies. Churchill called the rescue at Dunkirk a “miracle of deliverance,” well the miracle of Moderna will rescue many more. Not only was a vaccine designed in under a year, an entirely new production process was set up to produce billions of doses to rescue the world. The creation of the mRNA vaccines was a triumph of science, logistics, and management and it was done at a speed that I had thought possible only for past generations.
I am grateful that greatness is still within our civilization’s grasp.
Addendum: Lest I be accused of being reflexively pro-patent, do recall the Tabarrok curve.
India’s Pandemic and the World
Shruti Rajagopalan is right, helping India isn’t just about India.
India’s role in the global pandemic is unique. The developing world is counting on affordable Indian vaccine-makers such as Serum Institute of India Pvt. Ltd. for their supplies. With India now reserving virtually all its doses for domestic use, those countries will have to wait even longer to be vaccinated. And if the pandemic disrupts production at Indian pharmaceutical companies, it could affect crucial non-Covid medications as well. Half the world’s children have been vaccinated by Serum Institute.
The Biden administration can do two things to help. The first is to ease restrictions on critical exports, imposed under the Defense Production Act to prioritize the needs of U.S. companies.
Vaccine production requires very specific, medically approved inputs, which are difficult to substitute quickly in the middle of a pandemic. Currently, U.S. producers must secure permission before exporting such things as special sterile filters, disposable bags for cell cultures, cell culture media and single-use tubing. The embargo has led to major bottlenecks. Serum Institute says that without those inputs, it may not be able to deliver the 160 million vaccine doses it had planned to produce next month.
Second, the U.S. should immediately share doses from its own supply of Oxford-AstraZeneca and Johnson & Johnson vaccines.
I have three things to add. First, I have already noted the foreign policy implications which weigh strongly in favor of taking a more active role in the world pandemic.
Second, India should move immediately to delay the second dose of the AZ vaccine to 12 weeks. The federal government has already recommended a 6-8 week schedule, as this improves efficiency of the AstraZeneca (Covishield) vaccine, but many people so fear shortages that they are getting a less-effective second dose at four weeks. An enforced 12 week schedule would improve efficiency and might also reassure people that there will be supplies in 12 weeks.
Third, and this is more speculative, but the rising pandemic in India provides an opportunity to test fractional dosing of the Pfizer and Moderna vaccines in a real world setting. There is currently a small-scale Belgian trial testing Moderna at 50 mcg and Pfizer at 20 mcg. We already have reasonable information that 50 mcg of Moderna induces a robust immune response in adults. The mRNA vaccines wouldn’t work in all of India but would be fine in the cities and perhaps there is an opportunity for an exchange similar to what Israel promised to get early supplies.
Atul Gawande and Zeke Emanuel Now Support Delaying the Second Dose
Many people are coming around to First Doses First, i.e delaying the second dose to ~12 weeks. Atul Gawande, for example, tweeted:
As cases and hospitalizations rise again, we can’t count on behavior alone reversing this course. Therefore, it’s time for the Biden admin to delay 2nd vax doses to 12 weeks. Getting as many people as possible a vax dose is now urgent.
Now urgent??? Yes, I am a little frustrated because the trajectory on the new variants was very clear. On January 1, for example, I wrote about The New Strain and the Need for Speed (riffing off an excellent piece by Zeynep Tufekci). Still, very happy to have Gawande’s voice added to the cause. Also joining Gawande are the power trio of Govind Persad, William F. Parker and Ezekiel J. Emanuel who in an important op-ed write:
If we temporarily delay second doses …that is our best hope of quelling the fourth wave ignited by the B.1.1.7 variant. Because we did not start this strategy earlier, it is probably too late for Michigan, New York, New Jersey and the other Northeastern states. But it might be just in time for the South and California — the next places the more infectious strain will go if historical patterns repeat.
…Drug manufacturers selected the three- or four-week interval currently used between doses to rapidly prove efficacy in clinical trials. They did not choose such short intervals based on the optimal way of using the vaccines to quell a pandemic. While a three- or four-week follow-up is safe and effective, there is no evidence it optimizes either individual benefit or population protection.
…Some complain that postponing second doses is not “following the science.” But the scientific evidence goes far beyond what was shown in the original efficacy trials. Data from the United Kingdom, Israel and now the Centers for Disease Control and Prevention shows that first doses both prevent infection and reduce transmission. In people with prior infection, experts are beginning to recognize that a second dose could provide even less benefit. Following the science means updating policies to recognize new evidence rather than stubbornly maintaining the status quo.
Emanuel is on Biden’s COVID-19 task force so consider this op-ed running the flag up the flagpole. I predict Topol will fall next.
I would be surprised, however, if the US changes course now–too many people would then ask why didn’t we do this sooner?–but dose stretching is going to be important for the rest of the world. Why aren’t we doing more to investigate fractional dosing? Even if we went to half-doses on the second dose–the full second dose appears to be strong–that would still be a significant increase in total supply.
Addendum: I have argued for sending extra doses to Michigan and other hot spots such as NJ. Flood the zone! The Biden administration says no. Why? Production is now running well ahead of distribution as more than 50 million doses have been delivered but not administered. It would be a particularly good idea to send more single-shot J&J to reach hard to reach communities–one and done.
In praise of Alex Tabarrok
Here’s a question I’ve been mulling in recent months: Is Alex Tabarrok right? Are people dying because our coronavirus response is far too conservative?
I don’t mean conservative in the politicized, left-right sense. Tabarrok, an economist at George Mason University and a blogger at Marginal Revolution, is a libertarian, and I am very much not. But over the past year, he has emerged as a relentless critic of America’s coronavirus response, in ways that left me feeling like a Burkean in our conversations.
He called for vastly more spending to build vaccine manufacturing capacity, for giving half-doses of Moderna’s vaccine and delaying second doses of Pfizer’s, for using the Oxford-AstraZeneca vaccine, for the Food and Drug Administration to authorize rapid at-home tests, for accelerating research through human challenge trials. The through line of Tabarrok’s critique is that regulators and politicians have been too cautious, too reluctant to upend old institutions and protocols, so fearful of the consequences of change that they’ve permitted calamities through inaction.
Tabarrok hasn’t been alone. Combinations of these policies have been endorsed by epidemiologists, like Harvard’s Michael Mina and Brown’s Ashish Jha; by other economists, like Tabarrok’s colleague Tyler Cowen and the Nobel laureates Paul Romer and Michael Kremer; and by sociologists, like Zeynep Tufekci (who’s also a Times Opinion contributor). But Tabarrok is unusual in backing all of them, and doing so early and confrontationally. He’s become a thorn in the side of public health experts who defend the ways regulators are balancing risk. More than one groaned when I mentioned his name.
But as best as I can tell, Tabarrok has repeatedly been proved right, and ideas that sounded radical when he first argued for them command broader support now. What I’ve come to think of as the Tabarrok agenda has come closest to being adopted in Britain, which delayed second doses, approved the Oxford-AstraZeneca vaccine despite its data issues, is pushing at-home testing and permitted human challenge trials, in which volunteers are exposed to the coronavirus to speed the testing of treatments. And for now it’s working: Britain has vaccinated a larger percentage of its population than the rest of Europe and the United States have and is seeing lower daily case rates and deaths.
Dose Stretching Policies Probably *Reduce* Mutation Risk
One objection to dose-stretching policies, such as delaying the second dose or using half-doses, is that this might increase the risk of mutation. While possible, some immunologists and evolution experts are now arguing that dose-stretching will probably reduce mutation risk which is what Tyler and I concluded. Here’s Tyler:
One counter argument is that letting “half-vaccinated” people walk around will induce additional virus mutations. Florian Kramer raises this issue, as do a number of others.
Maybe, but again I wish to see your expected value calculations. And in doing these calculations, keep the following points in mind:
a. It is hard to find vaccines where there is a recommendation of “must give the second dose within 21 days” — are there any?
b. The 21-day (or 28-day) interval between doses was chosen to accelerate the completion of the trial, not because it has magical medical properties.
c. Way back when people were thrilled at the idea of Covid vaccines with possible 60% efficacy, few if any painted that scenario as a nightmare of mutations and otherwise giant monster swarms.
d. You get feedback along the way, including from the UK: “If it turns out that immunity wanes quickly with 1 dose, switch policies!” It is easy enough to apply serological testing to a control group to learn along the way. Yes I know this means egg on the face for public health types and the regulators.
e. Under the status quo, with basically p = 1 we have seen two mutations — the English and the South African — from currently unvaccinated populations. Those mutations are here, and they are likely to overwhelm U.S. health care systems within two months. That not only increases the need for a speedy response, it also indicates the chance of regular mutations from the currently “totally unvaccinated” population is really quite high and the results are really quite dire! If you are so worried about hypothetical mutations from the “half vaccinated” we do need a numerical, expected value calculation comparing it to something we already know has happened and may happen yet again. When doing your comparison, the hurdle you will have to clear here is very high.
(See my Washington Post piece for similar arguments and additional references.).
Now here are evolutionary theorists, immunologists and viral experts Sarah Cobey, Daniel B. Larremore, Yonatan H. Grad, and Marc Lipsitch in an excellent paper that first reviews the case for first doses first and then addresses the escape argument. They make several interrelated arguments that a one-dose strategy will reduce transmission, reduce prevalence, and reduce severity and that all of these effects reduce mutation risk.
The arguments above suggest that, thanks to at least some effect on transmission from one dose, widespread use of a single dose of mRNA vaccines will likely reduce infection prevalence…
The reduced transmission and lower prevalence have several effects that individually and together tend to reduce the probability that variants with a fitness advantage such as immune escape will arise and spread (Wen, Malani, and Cobey 2020). The first is that with fewer infected hosts, there are fewer opportunities for new mutations to arise—reducing available genetic variation on which selection can act. Although substitutions that reduce antibody binding were documented before vaccine rollout and are thus relatively common, adaptive evolution is facilitated by the appearance of mutations and other rearrangements that increase the fitness benefit of other mutations (Gong, Suchard, and Bloom 2013; N. C. Wu et al. 2013; Starr and Thornton 2016). The global population size of SARS-CoV-2 is enormous, but the space of possible mutations is larger, and lowering prevalence helps constrain this exploration. Other benefits arise when a small fraction of hosts drives most transmission and the effective reproductive number is low. Selection operates less effectively under these conditions: beneficial mutations will more often be lost by chance, and variants with beneficial mutations are less certain to rise to high frequencies in the population (Desai, Fisher, and Murray 2007; Patwa and Wahl 2008; Otto and Whitlock 1997; Desai and Fisher 2007; Kimura 1957). More research is clearly needed to understand the precise impact of vaccination on SARS-CoV-2 evolution, but multiple lines of evidence suggest that vaccination strategies that reduce prevalence would reduce rather than accelerate the rate of adaptation, including antigenic evolution, and thus incidence over the long term.
In evaluating the potential impact of expanded coverage from dose sparing on the transmission of escape variants, it is necessary to compare the alternative scenario, where fewer individuals are vaccinated (but a larger proportion receive two doses) and more people recover from natural infection. Immunity developing during the course of natural infection, and the immune response that inhibits repeat infection, also impose selection pressure. Although natural infection involves immune responses to a broader set of antibody and T cell targets compared to vaccination, antibodies to the spike protein are likely a major component of protection after either kind of exposure (Addetia et al. 2020; Zost et al. 2020; Steffen et al. 2020), and genetic variants that escape polyclonal sera after natural infection have already been identified (Weisblum et al. 2020; Andreano et al. 2020). Studies comparing the effectiveness of past infection and vaccination on protection and transmission are ongoing. If protective immunity, and specifically protection against transmission, from natural infection is weaker than that from one dose of vaccination, the rate of spread of escape variants in individuals with infection-induced immunity could be higher than in those with vaccine-induced immunity. In this case, an additional advantage of increasing coverage through dose sparing might be a reduction in the selective pressure from infection-induced immunity.
…In the simplest terms, the concern that dose-sparing strategies will enhance the spread of immune escape mutants postulates that individuals with a single dose of vaccine are those with the intermediate, “just right” level of immunity, more likely to evolve escape variants than those with zero or two doses (Bieniasz 2021; Saad-Roy et al. 2021)….There is no particular reason to believe this is the case. Strong immune responses arising from past infection or vaccination will clearly inhibit viral replication, preventing infection and thus within-host adaptation…. Past work on influenza has found no evidence of selection for escape variants during infection in vaccinated hosts (Debbink et al. 2017). Instead, evidence suggests that it is immunocompromised hosts with prolonged influenza infections and high viral loads whose viral populations show high diversity and potentially adaptation (Xue et al. 2017, 2018), a phenomenon also seen with SARS-CoV-2 (Choi et al. 2020; Kemp et al. 2020; Ko et al. 2021). It seems likely, given its impact on disease, that vaccination could shorten such infections, and there is limited evidence already that vaccination reduces the amount of virus present in those who do become infected post-vaccination (Levine-Tiefenbrun et al. 2021).
I also very much agree with these more general points:
The pandemic forces difficult choices under scientific uncertainty. There is a risk that appeals to improve the scientific basis of decision-making will inadvertently equate the absence of precise information about a particular scenario with complete ignorance, and thereby dismiss decades of accumulated and relevant scientific knowledge. Concerns about vaccine-induced evolution are often associated with worry about departing from the precise dosing intervals used in clinical trials. Although other intervals were investigated in earlier immunogenicity studies, for mRNA vaccines, these intervals were partly chosen for speed and have not been completely optimized. They are not the only information on immune responses. Indeed, arguments that vaccine efficacy below 95% would be unacceptable under dose sparing of mRNA vaccines imply that campaigns with the other vaccines estimated to have a lower efficacy pose similar problems. Yet few would advocate these vaccines should be withheld in the thick of a pandemic, or roll outs slowed to increase the number of doses that can be given to a smaller group of people. We urge careful consideration of scientific evidence to minimize lives lost.