How Much Did Physicians Drive the Opioid Crisis?
It’s well known that the opioid crisis started with prescription abuse but how much abuse was driven by patients who fooled their physicians and how much was driven by physicians who responded to monetary incentives with a nod and a wink? Molly Schnell provides some evidence which even a hard headed rationalist like myself found startling.
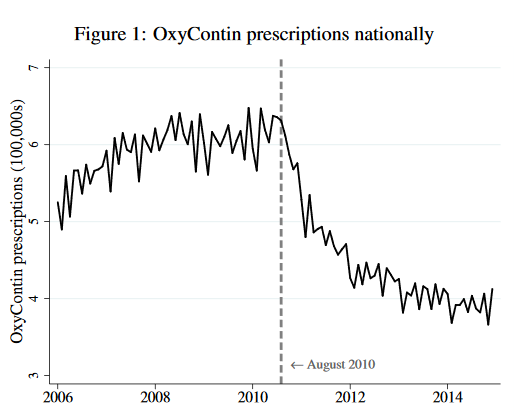 In August of 2010, Purdue Pharma replaced old OxyContin with a new, anti-abuse version of OxyContin. The new version was just as good at reducing pain as the old but it was more difficult to turn it into an injectable to produce a high. If physicians are altruists who balance treating their patient’s pain against their fear of patient addiction and downstream abuse then they should increase their prescriptions of new Oxy. From the point of view of health, the new Oxy is simply a better drug and with less abuse to worry about altruistic physicians should be more willing on the margin to prescribe Oxy to reduce pain. So what happened? Prescriptions for Oxy fell immediately and dramatically when the better version was released.
In August of 2010, Purdue Pharma replaced old OxyContin with a new, anti-abuse version of OxyContin. The new version was just as good at reducing pain as the old but it was more difficult to turn it into an injectable to produce a high. If physicians are altruists who balance treating their patient’s pain against their fear of patient addiction and downstream abuse then they should increase their prescriptions of new Oxy. From the point of view of health, the new Oxy is simply a better drug and with less abuse to worry about altruistic physicians should be more willing on the margin to prescribe Oxy to reduce pain. So what happened? Prescriptions for Oxy fell immediately and dramatically when the better version was released.
Now, to be fair to the physicians, patients who wanted to abuse Oxy stopped demanding it after the new version was released and physicians might not have realized how many of their prescriptions were being abused or sold on the secondary market. The aggregate data, which is a combination of supply and demand shifts, can mask individual physician behavior. Schnell, however, has data on the prescribing behavior of about 100,000 individual physicians who prescribed opioids.
Schnell finds that nearly a third of physicians behaved exactly as the altruism theory predicts. Namely, when new Oxy was released these altruistic physicians increased their prescriptions of Oxy and they maintained or reduced their prescriptions of other opioids. In fact, the median altruistic physician doubled their prescriptions of the new and improved Oxy. But almost 40% of physicians in Schnell’s sample behaved in a decidedly non-altruistic manner. Beginning in August of 2010, these non-altruistic physicians halved their prescriptions of new and improved Oxy and increased their prescriptions of other opioids. It’s difficult to see how attentive and altruistic physicians could decrease their demand for a better drug.
Schnell also finds that some parts of the country had fewer altruistic physicians and the consequences are evident in mortality statistics:
…. these differences in physician altruism across commuting zones translate into significant differences in mortality across locations…a one standard deviation increase in low-altruism physicians is associated with a 0.33 standard deviation increase in deaths involving drugs per capita. While this association is reduced conditional on observable commuting zone characteristics (including race, age, education, and income profiles), a significant and large association between the share of low-altruism physicians and drug-related mortality remains. Furthermore…this relationship persists even conditional on the number of opioid prescriptions, suggesting that the association is driven by the allocation of prescriptions introduced by low-altruism physicians rather than simply the quantity.
The less-altruistic physicians increased prescriptions for other opioids after new Oxy was introduced but perhaps even this was better than the non-prescription alternatives like heroin and street fentanyl. Indeed, Alpert, Powell and Pacula show that the introduction of improved Oxy led to more deaths because people switched to more dangerous, illegal alternatives. So was it a bad idea to introduce a better drug? Maybe, but if new Oxy had been introduced earlier perhaps fewer people would have been addicted, leading to less demand for illegal markets later. Thus, static and dynamic effects may differ. The economics of dual use goods is complicated.