Category: Medicine
What should I ask David Cutler?
He has a new book out with Ed Glaeser, namely Survival of the City: Living and Thriving in an Age of Isolation.
I will be doing a joint CWT with them, sequentially rather than simultaneous. So what should I ask David Cutler? There is a separate post for suggestions for Glaeser.
A reader’s wishes for Covid coverage
From my email:
“In the last 18-19 months why have these stories not been written:
• Why no stories on hospice care in the United States relating to covid19 statistics (hospice has been removed from our common lexicon)? I’ve asked you this before, I know.
• Why no stories on the earnings of publicly held life insurance companies ?
• Why no stories about strategies written about the myriad of home health care providers in this country? What is their role in lessening hospital stays in the last 18 months. Did they play a role?
• Why know detailed explanation of how excess deaths are calculated – what are the excess death estimates for the next 5 years? I assume the data is easily found.
• No actuaries providing keen information and insights?
• Detailed investigations and stories of the traveling nurse industry ? I know several, interesting stories to say the least. Mostly regarding compensation.
• No keen insights from the coroners industry? The inexact science of “cause of death” in the last 100 years.
Would love you thoughts on my questions and why have there been no stories about the above?”
Fluvoxamine update and new call for related proposals
In December 2020, we noticed a few findings — some of them from Fast Grants-funded scientists — that led us to be optimistic that fluvoxamine might be an effective Covid-19 treatment.
— Patrick Collison (@patrickc) August 16, 2021
Do read through the whole thread!
The FDA and CDC Standards on the J&J Vaccine and the Immunocompromised are Unintelligible
Last week the FDA authorized and the CDC now recommends a third mRNA booster for the immunocomprimised. The CDC says:
Who Needs an Additional COVID-19 Vaccine?
Currently, CDC is recommending that moderately to severely immunocompromised people receive an additional dose. This includes people who have:
- Been receiving active cancer treatment for tumors or cancers of the blood
- Received an organ transplant and are taking medicine to suppress the immune system
- Received a stem cell transplant within the last 2 years or are taking medicine to suppress the immune system
- Moderate or severe primary immunodeficiency (such as DiGeorge syndrome, Wiskott-Aldrich syndrome)
- Advanced or untreated HIV infection
- Active treatment with high-dose corticosteroids or other drugs that may suppress your immune response
That’s very reasonable but the headline is inaccurate because the CDC then goes on to say:
The FDA’s recent EUA amendment only applies to mRNA COVID-19 vaccines, as does CDC’s recommendation.
Emerging data have demonstrated that immunocompromised people who have low or no protection following two doses of mRNA COVID-19 vaccines may have an improved response after an additional dose of the same vaccine. There is not enough data at this time to determine whether immunocompromised people who received the Johnson & Johnson’s Janssen COVID-19 vaccine also have an improved antibody response following an additional dose of the same vaccine.
So if you got one dose of J&J and are immunocompromised then you can’t get a second dose. But if you got two doses of an mRNA (which is already more effective than one dose of J&J) and are immunocompromised then the CDC recommends a third dose. None of this makes any sense. The weasel words there ‘isn’t enough data to determine’ indicate a typical failure to think in Bayesian terms and use all the information available and a typical failure to think in terms of patient welfare and expected cost and benefits.
Notice also the illiberal default. Instead of saying ‘we don’t have data on the J&J vaccine and the immunocompromised so we are not at this time recommending or not recommending boosters but leaving this decision in the hands of patients and their physicians’ they say ‘we don’t have data and so we are forbidding patients and their physicians from making a decision using their own judgment.’
Hat tip: Pharmacist CB.
This should be hailed, and yet there is mostly silence from the elites
Florida Gov. Ron DeSantis rolled out a new state treatment plan to help fight COVID-19, announcing Thursday that the state will start dispensing Regeneron monoclonal antibodies through mobile clinics…
DeSantis is urging people at high risk — the elderly, the obese, people with diabetes — to get the monoclonal antibodies at the first indication of COVID-19.
Florida is making the antibody therapies more widely available by opening a rapid response unit in Jacksonville with an eye toward expanding across the state.
Here is the full story.
Fluvoxamine seems to work against Covid-19
🚨Interim results of @TogetherTrial of ivermectin and fluvoxamine for early treatment of #COVID_19 🚨#ivermectin : no significant effect#fluvoxamine: ↘️ risk of hospitalization by 31%
These important results deserve a🧵 1/n https://t.co/oSy1p91hs2— Julien Potet (@julienpotet) August 12, 2021
That is from a project funded by Fast Grants.
Our Regulatory State Isn’t Learning
Delta is the fourth wave of covid, and amazingly the US policy response is even more irresolute than the first time around. Our government is like a child, sent next door to get a cup of sugar, who gets as far as the front stoop and then wanders off following a puppy.
The policy response is now focused on the most medically ineffective but most politically symbolic step, mask mandates. An all-night disco in Provincetown turns in to a superspreader event so… we make school kids wear masks in outdoor summer camps? Masks are several decimal places less effective than vaccines, and less effective than “social distance” in the first place.* Go to that all night disco, unvaccinated, but wear a mask? Please.
If we’re going to do NPI (non pharmaceutical interventions), policy other than vaccines, the level of policy and public discussion has tragically regressed since last summer. Last summer, remember, we were all talking about testing. Alex Tabarrok and Paul Romer were superb on how fast tests can reduce the reproduction rate, even with just voluntary isolation following tests. Other countries had competent test and tracing regimes. Have we built that in a year? No. (Are we ready to test and trace the next bug? Double no.)
What happened to the paper-strip tests you could buy for $2.00 at Walgreen’s, get instant results, and maybe decide it’s a bad idea to go to the all night dance party? Interest faded in November. (Last I looked, the sellers and FDA were still insisting on prescriptions and an app sign up, so it cost $50 and insurance “paid for” it.) What happened to detailed local data? Did anyone ever get it through the FDA’s and CDCs thick skulls that even imperfect but cheap and fast tests can be used to slow spread of disease?
…And then we indulge another round of America’s favorite pastime, answers in search of a question. Delta is spreading, so… extend the renter eviction moratorium. People who haven’t paid rent in a year can stay, landlords be damned.
All true. I got dispirited on testing. It’s insane that we don’t have cheap, rapid testing and good ventilation ready for a new school year. As I wrote about earlier, even the American Academy of Pediatrics is shouting from the rooftops that the FDA is deadly slow. The eviction moratorium is a sick joke. Just a backhanded way to redistribute wealth without a shred of justice or reason. Disgusting.
Here’s one more bit (but read the whole thing there is more.)
To learn from the mistakes, and institutionalize better responses would mean to admit there were mistakes. One would think the grand blame-Trump-for-everything narrative would allow us to do that, but the mistakes are deeply embedded in the bureacracies of the administrative state. Unlike bad admirals in WWII, nobody less than Trump himself has lost their job over incompetent covid response. The institutions have an enormous investment in ratifying that they did the best possible job last time. So, as in so many things (financial bailouts!) we institutionalize last time’s mistakes to keep those who made them in power in power — which means we do not learn from mistakes.
Covid dispatch from a relatively non-Straussian country
Most people will end up contracting the coronavirus, the head of the Health Ministry’s advisory committee for infectious diseases predicted on Monday.
“The [real] question is whether the infected person is vaccinated or not. It’s unavoidable that the pandemic will infect the majority of the population. It won’t disappear in another half a year,” Dr. Tal Brosh told the Kan public broadcaster.
Brosh, who also heads the infectious disease department at Assuta Medical Center in Ashdod, said he doesn’t see a reason to shutter Ben Gurion Airport, arguing that would distract “from the main problem — morbidity within in the country.”
WWAFS? How many of our mainstream public health experts would even consider addressing such a question at this point? Do you think they are telling you the truth?
p.s. Which again is the country with the best data?
Addended p.p.s.: “Between 90% and 94% of British adults have some degree of immunity to coronavirus from full or partial vaccination, or prior infection, the U.K. statistics office estimates, based on statistical analysis of blood samples.”
Here is the full story. Via Rich B.
At this point, do you wish to simply not look too closely at the Delta data?
The delta Straussians also don’t want to debate safety claims very much. They fear that studying the data more closely will worry and paralyze us more, without much limiting the overall number of infections. In their view, vaccines have made things about as safe as they are going to get, and the contagiousness of delta will create lots of infections, albeit mostly relatively safe ones.
That’s what the proprietor of one of my favorite local restaurants believes. He is aware of the delta strain, and knows it is worse, though without being up on the numbers or the details. Earlier in the summer, he lifted the mask mandate for his restaurant, and he isn’t interested in restoring it. He is not a “Covid denialist,” but he figures normal business has to continue at some point and that point is now. Someone may well catch Covid in his restaurant, but those people might well have caught Covid anyway.
Our school reopenings face a similar paralysis-inducing dilemma. If we test every child every day, it will seem as if we have far too many cases of Covid, and the schools will shut again quickly. Nonetheless, given that delta is highly contagious, many of those children will catch Covid whether or not they go to school…
I do not rue the growth of delta Straussianism among my fellow citizens. If you can’t do anything about delta, if your institution needs to reopen sooner or later, if the booster shots in large numbers are not right around the corner, and yet another new variant might be coming along anyway, maybe you really do just need to get on with things. Restaurant reservations are robust, and the gym industry is surging back. I do not wish to reverse those trends, and it is hard to believe those customers are only the Covid denialists.
Here is the full Bloomberg column, which also offers a take on the British test and trace system.
Don’t judge Covid conditions by the current rate of Covid growth
These days when I go to Twitter I see so many claims that current caseload or hospitalization numbers (in some not all regions) are approaching their peaks from the third wave last winter.
But don’t be misled by that rhetoric — speed of growth is not at this stage of the pandemic a good metric for evaluation. Obviously, speedy Covid growth is bad news compared to having no Covid at all, but relative to actual constraints inference here is difficult. Even the growth of hospitalizations, much less the growth in cases, is a misleading signal for how well we are doing.
First, there is a diehard core of individuals who just won’t get vaccinated. That is highly unfortunate, but possibly it is better if those individuals get Covid sooner rather than later, at least provided they are not so numerous as to overwhelm the hospital system all at once. The Covid case is in essence their preferred form of vaccination. Stupid, yes, but later is not necessarily better.
A second possibility is that we will see waves of Delta Covid, rising rapidly and then declining rapidly. That seemed to happen in the most badly afflicted parts of India, and maybe has been happening in England and the Netherlands, noting that the English numbers have begun a recent (minor?) uptick again, so we cannot be sure of the dynamics. The general point stands that it is better to get a given amount of Covid over with more quickly rather than less quickly, again subject to the constraint that you do not overwhelm your hospital system. Circa August 2021, we are no longer in the older position of “waiting for the vaccines to arrive.”
A third possibility is that Delta really is extremely contagious and that non-pharmaceutical interventions just aren’t going to succeed in checking it. (Oddly, few elites are willing to mention this possibility. Though they are willing to tell us how terrible it is, which it is!) Yes, boosters may help out, but most of the “cavalry” — vaccines in this case — already has arrived, at least for those willing to take them. OK, so if most people are going to be hit by this thing, and vaccinations do make that event much safer than before, again you want to get that process over with more quickly rather than less quickly. And to the extent vaccine protection decays (an unknown variable but a real worry), speed really is of the essence here. Again, all subject to the “don’t overwhelm your hospital system” caveat.
Clearly there are scenarios where the rapid case growth is a bad thing, even taking relevant constraints into account. For instance, vaccinating younger individuals might be a relevant “cavalry” still to arrive, and maybe it can arrive before most of our young people are exposed to Covid. Or maybe most of the unvaccinated are pretty “elastic” in their status, and a high but not too high case and hospitalization growth will scare them enough to bring them over to the vaccinated side of the ledger. Those really are possibilities.
But rapid growth per se — even on the hospitalization side of the ledger — has to be used with care as an indicator of where we stand. Generating a lot of Covid cases and hospitalizations in a short period of time is a very tricky signal, again relative to the constraints we face. You need to define your counterfactual very carefully, and recognize that the mood affiliations you were promoting earlier in the pandemic may or may not make sense now.
The performance of the NIH during the pandemic in 2020
“A new research study by one of us and his Johns Hopkins colleagues found that of the $42 billion the National Institutes of Health spent on research last year, less than 2% went to Covid clinical research…
Here is the WSJ source. Here is the full report from Johns Hopkins, and here is the executive summary:
● Of the $42 Billion 2020 NIH annual budget, 5.7% was spent on
COVID-19 research
● Public health research was underfunded at 0.4% of the 2020 NIH
budget
● Only 1.8% of the 2020 NIH budget was spent on COVID-19 clinical
research
● Average COVID-19 NIH funding cycle was 5 months
● Aging was funded 2.2 times more than COVID-19 research
● By May 1, 2020, 3 months into the pandemic, the NIH spent 0.05%
annual budget on COVID-19 research
● Of the 1419 grants funded by the NIH:
• NO grants on kids and masks specifically
• 58 studies on social determinants of health
• 57 grants on substance abuse
• 107 grants on developing COVID-19 medications
• 43 of the 107 medication grants repurposed existing drugs
Ouch. Here is a not entirely random sentence from the report:
The COVID-19 pandemic has only exacerbated the NIH institutional challenges and inability to reallocate funds quickly to
critical research.
Here is another damning sentence, though it damns someone other than the NIH:
…to date, no research has investigated NIH COVID-19 funding patterns to the best of our knowledge.
Double ouch. Might the NIH have too much influence over the allocation of funds to be investigated properly? Rooftops, people…
The American Academy of Pediatrics Tells the FDA to Speed Up and Stop Endangering Patients
 The American Academy of Pediatrics has written a stunning letter to the FDA:
The American Academy of Pediatrics has written a stunning letter to the FDA:
We understand that the FDA has recently worked with Pfizer and Moderna to double the number of children ages 5-11 years included in clinical trials of their COVID-19 vaccines. While we appreciate this prudent step to gather more safety data, we urge FDA to carefully consider the impact of this decision on the timeline for authorizing a vaccine for this age group. In our view, the rise of the Delta variant changes the risk-benefit analysis for authorizing vaccines in children. The FDA should strongly consider authorizing these vaccines for children ages 5-11 years based on data from the initial enrolled cohort, which are already available, while continuing to follow safety data from the expanded cohort in the post-market setting. This approach would not slow down the time to authorization of these critically needed vaccines in the 5–11-year age group.
In addition, as FDA continues to evaluate clinical trial requirements for children under 5 years, we similarly urge FDA to carefully consider the impact of its regulatory decisions on further delays in the availability of vaccines for this age group. Based on scientific data currently available on COVID-19 vaccines, as well as on 70 years of vaccinology knowledge in the pediatric population, the Academy believes that clinical trials in these children can be safely conducted with a 2-month safety follow-up for participants. Assuming that the 2-month safety data does not raise any new safety concerns and that immunogenicity data are supportive of use, we believe that this is sufficient for authorization in this and any other age group. Waiting on a 6-month follow-up will significantly hinder the ability to reduce the spread of the hyper infectious COVID-19 Delta variant among this age group, since it would add 4 additional months before an authorization decision can be considered. Based on the evidence from the over 340 million doses of COVID-19 doses administered to adults and adolescents aged 12-17,as well as among adults 18 and older, there is no biological plausibility for serious adverse immunological or inflammatory events to occur more than two months after COVID-19 vaccine administration.
In my many years of writing about the FDA, I can’t recall a single instance in which a major medical organization told the FDA to use a smaller trial and speed up the process because FDA delay was endangering the safety of their patients. Wow.
The invisible graveyard is invisible no more.
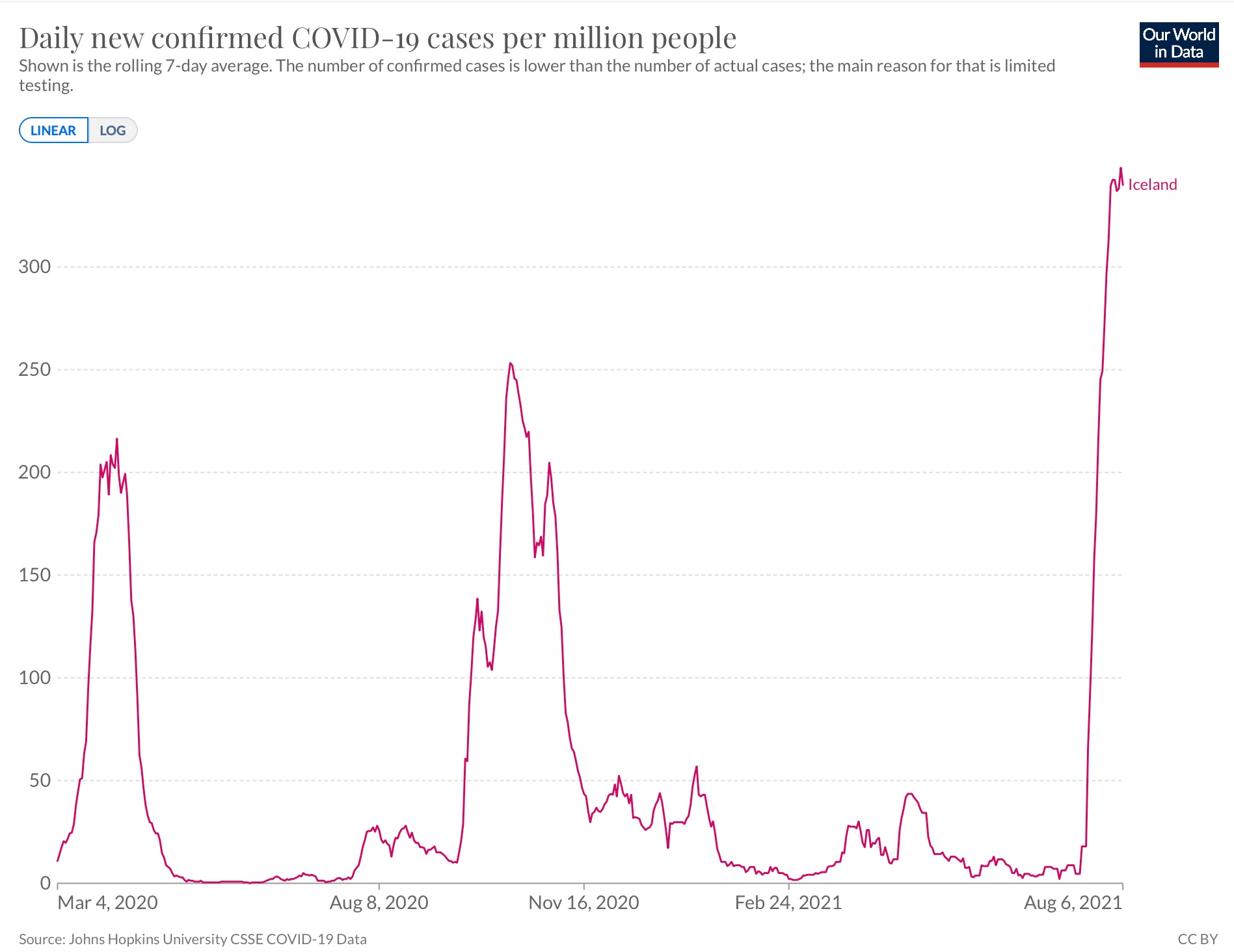
Iceland and Covid
As you may know, Iceland is one of the most fully vaccinated countries in the world:
All via Eric Topol. No, I am not arguing we should give up or stop looking for policy and most of all biomedical improvements. All the more reason to do so! But…this does indicate we will need to find some way of living with such case numbers, without falling apart and pulling the plug on economic activity.
Masks and the Delta variant
I haven’t seen any systematic, data-based investigation of how well cloth masks work against the Delta variant, and it is too early to expect it. Nonetheless I tried to do some simple mental modeling of my own.
We do know that the viral load from Delta is much higher. That could make masks less effective, because perhaps they cannot stop the spewer from spreading the virus so easily. (Oddly, you don’t see many people admitting such an effect might be possible, as this seems to be a politically incorrect idea to present.)
Yet there is a countervailing factor. The Delta variant spreads far more rapidly than “classic Covid.” So a given “small effect” of a mask is more important. It used to be that a mask (sometimes) stopped the spread to one person, who in turn might spread to 1.3 others. Now, if your mask stops the spread to that person, it might be stopping the subsequent spread to seven other people (we don’t know the exact number, but yes I have heard “seven” bandied around as a possibility).
To be clear, in this scenario masks are still less effective than before in preventing Covid spread. But the rate of return on wearing a mask, relative to no mask, can be higher. It is simply that the whole curve has shifted downward in a disadvantageous way. But if the mask has any effectiveness at all, that effectiveness is now magnified greatly.
Under some plausible numbers the protective potency of wearing a mask might be about five times higher (seven divided by recent non-Delta R, or something like that). Unless masks are five times (or more) less effective in stopping spread, masking could become more important rather than less important.
But the net effect could go either way.
That said, seeing other people masked should make you feel less secure than it used to. The new potential upside “rate of return effect” from masking is choking off the greater second order effects of the more rapid spread. The “are you going to get Covid from this particular masked person near you?” calculus seems to be decidedly worse than before.
The FDA Is Still Much Too Strict
Here is just one bit from a superb post on the FDA by psychiatrist Scott Alexander at Astral Codex Ten.
I worry that people are going to come away from this with some conclusion like “wow, the FDA seemed really unprepared to handle COVID.” No. It’s not that specific. Every single thing the FDA does is like this. Every single hour of every single day the FDA does things exactly this stupid and destructive, and the only reason you never hear about the others is because they’re about some disease with a name like Schmoe’s Syndrome and a few hundred cases nationwide instead of something big and media-worthy like coronavirus. I am a doctor and sometimes I have to deal with the Schmoe’s Syndromes of the world and every f@$king time there is some story about the FDA doing something exactly this awful and counterproductive.
A while back I learned about Infant Short Bowel Syndrome, a rare condition with only a few hundred cases nationwide. Babies cannot digest food effectively, but you can save their lives by using an IV line to direct nutrients directly into their veins. But you need to use the right nutrient fluid. The FDA approved an early draft of the nutrient fluid, but it didn’t have enough fish oil, which is necessary for development, so a lot of the babies still died or ended up with permanent neurological damage. Around the late 90s/early 00s, researchers figured out what was going on and recommended adding fish oil to the IV fluid. The FDA responded that they had only approved the non-fish-oil version, it would take them a while to approve the new version, and until they did that adding fish oil was illegal. A bunch of babies kept dying and getting permanent neurological damage, and everyone knew exactly how to stop it, but if anyone did the FDA would take away their licenses and shut them down. Around 2010, Boston Children’s Hospital found some loophole that let them add fish oil to their nutrient fluid on site, and infants with short bowel syndrome at that one hospital stopped dying or ending up permanently disabled, and the FDA grudgingly agreed to permit it but banned them from distributing their formulation or letting it cross state lines – so for a while if you wanted your baby not to die you had to have them spend their infancy in one specific hospital in Massachusetts. Around 2015 the FDA said that if your doctor applied for a special exemption, they would let you import the correct nutritional fluid from Europe (where, lacking the FDA, they had just added fish oil to the fluid as soon as researchers discovered it was necessary), but you were only able to apply after your baby had already sustained serious damage, and the FDA might just say no. Finally in 2018 the FDA got around to approving the corrected nutritional fluid and now babies with short bowel syndrome do fine, after twenty years of easily preventable state-mandated deaths. And it’s not just this and coronavirus, I CANNOT STRESS ENOUGH HOW TYPICAL THIS IS OF EVERYTHING THE FDA DOES ALL THE TIME.
Read the whole thing! I actually had to read it in several sessions, it’s not that long but bouts of anger interspersed with moments of laughter made me have to put it down momentarily to recover. There is a lot more in the post on reforms.
Best quick intro to my views on the FDA is this post (follow the links) and my paper on off-label prescribing.
Addendum: Scott updates the infant fish oil story and provides much more detail. He got some things wrong and the FDA as an agency ends up looking better but the broad outline about the FDA system looks right. I am leaving the post up for posterity but this specific part isn’t correct.